Early Detection of Pancreatic Cancer:
Newly Diagnosed Type 2 Diabetes
Early Detection of Pancreatic Cancer:
Newly Diagnosed Type 2 Diabetes
Pancreatic cancer is the third leading cause of cancer-related death and is predicted to be the second most common cause by 2030.1,2
~66,440 adults diagnosed in 20243
~51,750 deaths in the US in 20243
The impact of a silent killer
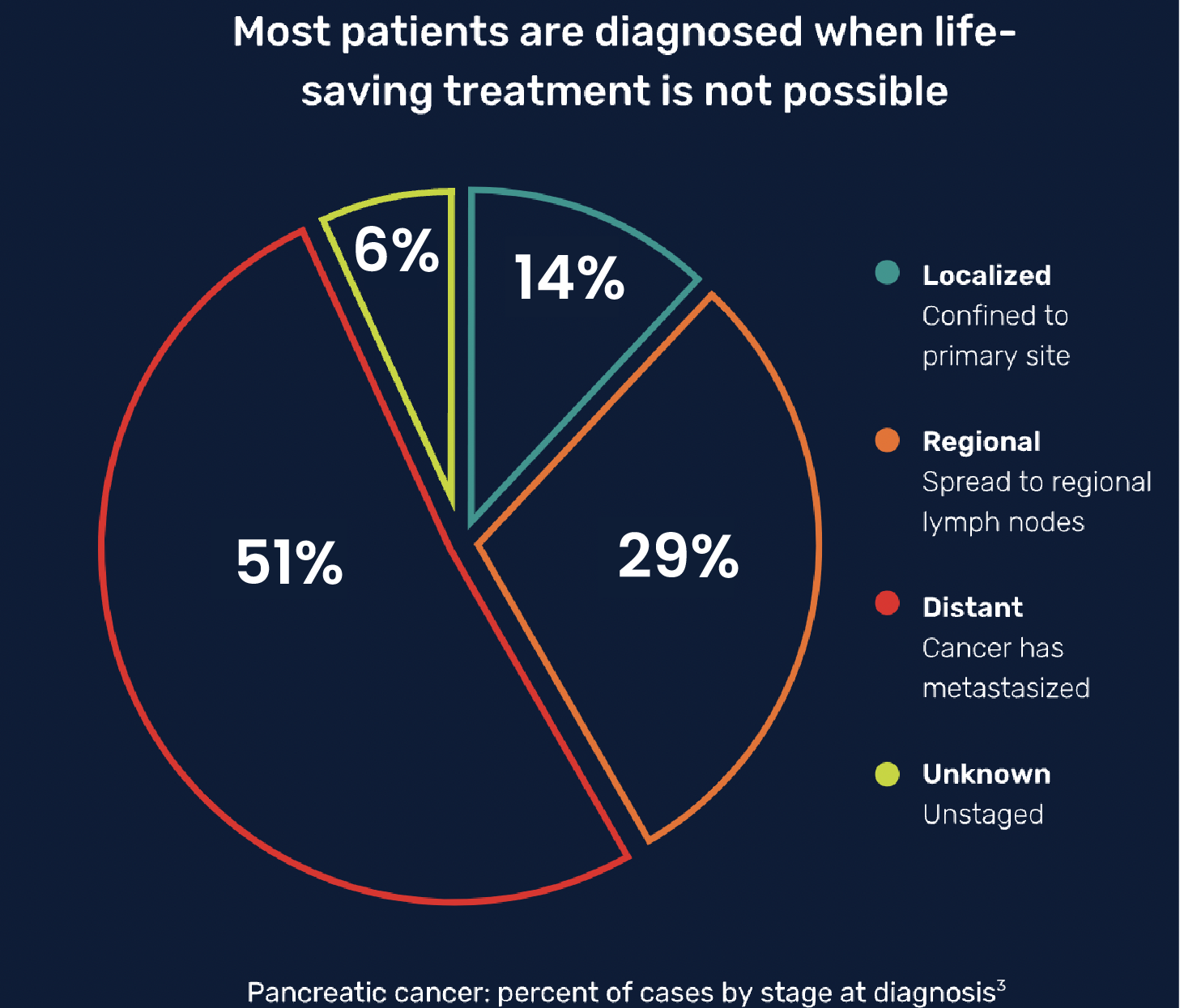
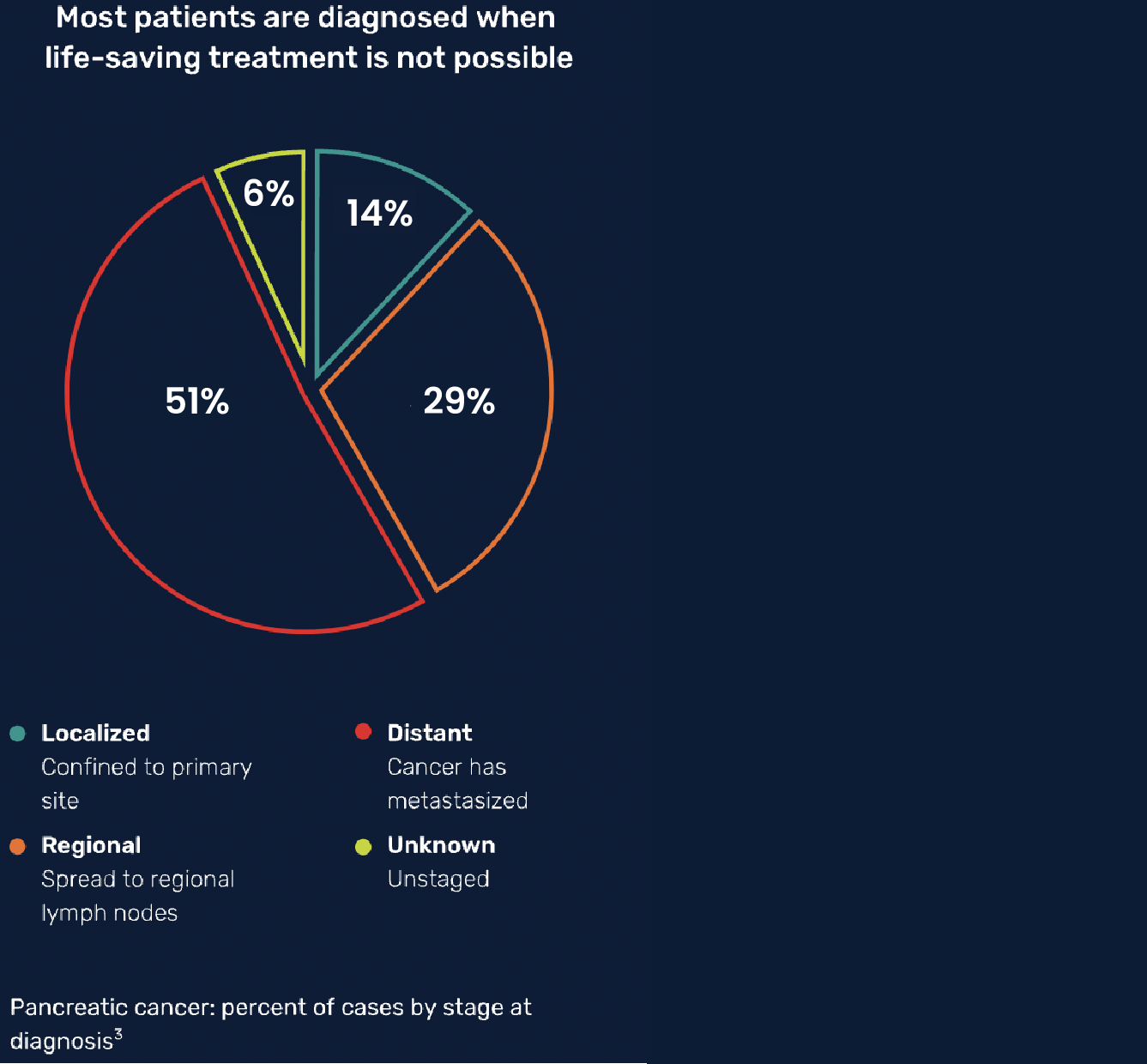
In pancreatic cancer, the vast majority of patients are not diagnosed until their cancer has advanced and they have regional (stage III) or distant (stage IV) tumors.3 For these patients, the prognosis is poor.

The potential benefit of early detection of pancreatic cancer patients
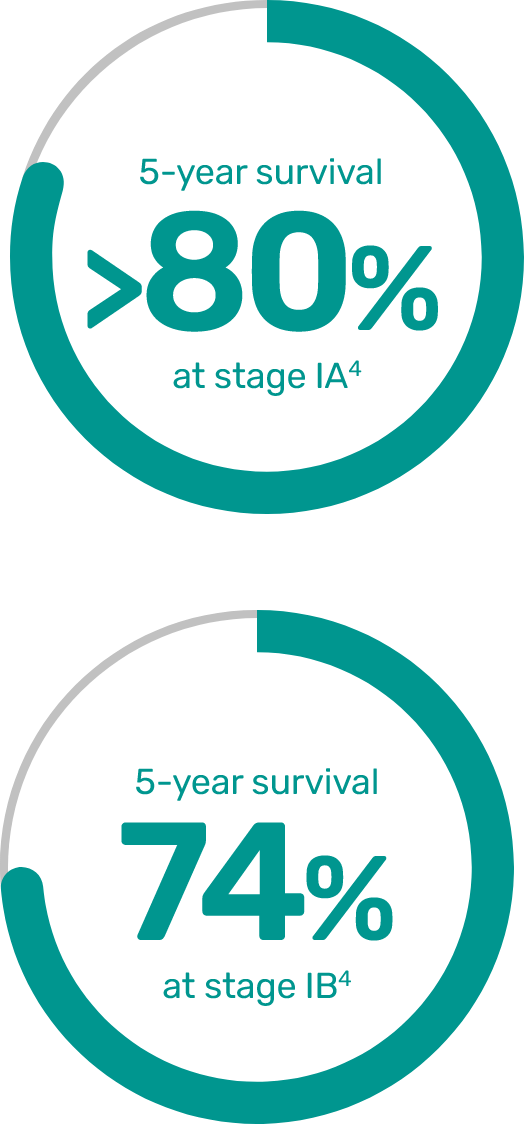
The stage of pancreatic cancer at diagnosis has a significant impact on survival.2 Pancreatic cancer diagnosed at its earliest stage (IA) can have a 5-year survival rate of over 80%.4
Identifying patients at high risk for pancreatic cancer
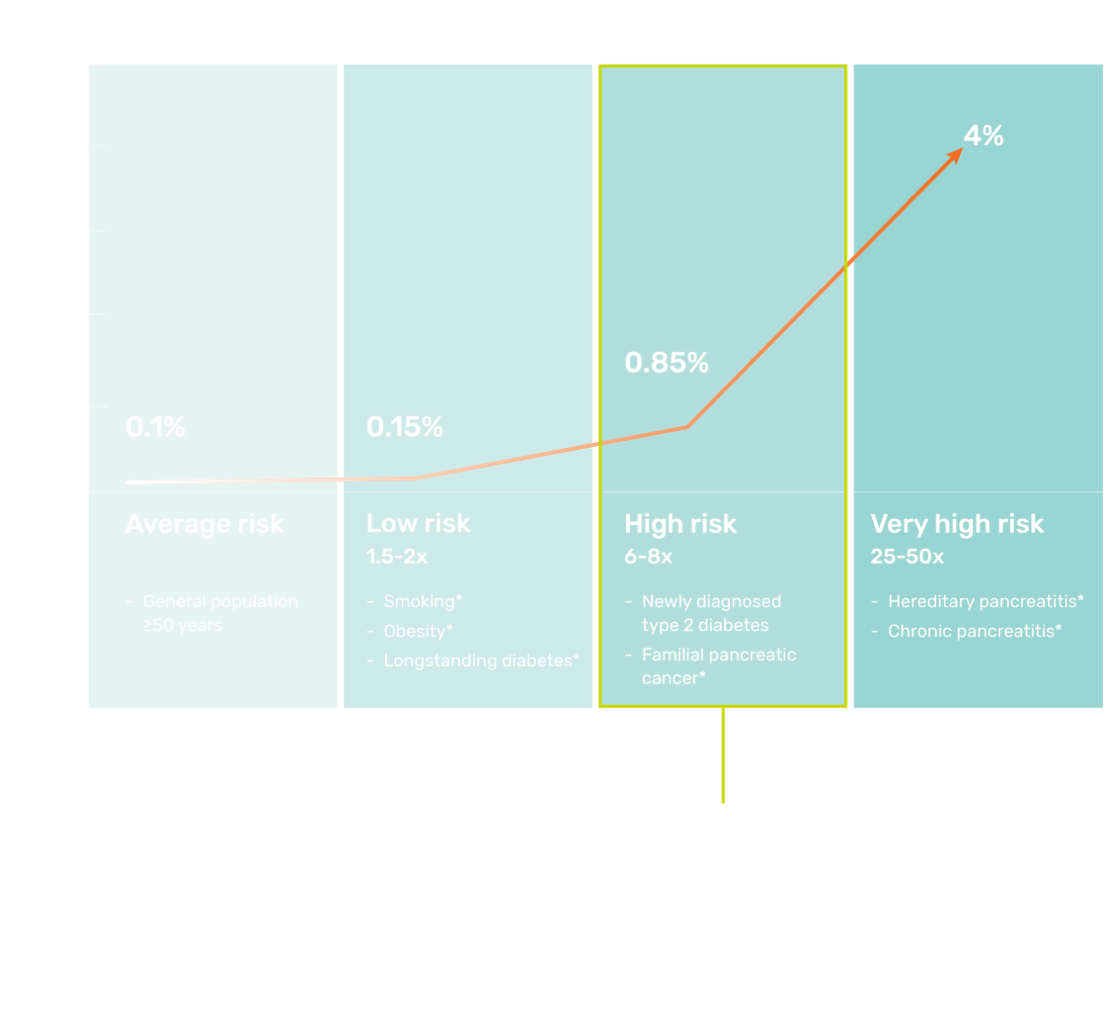
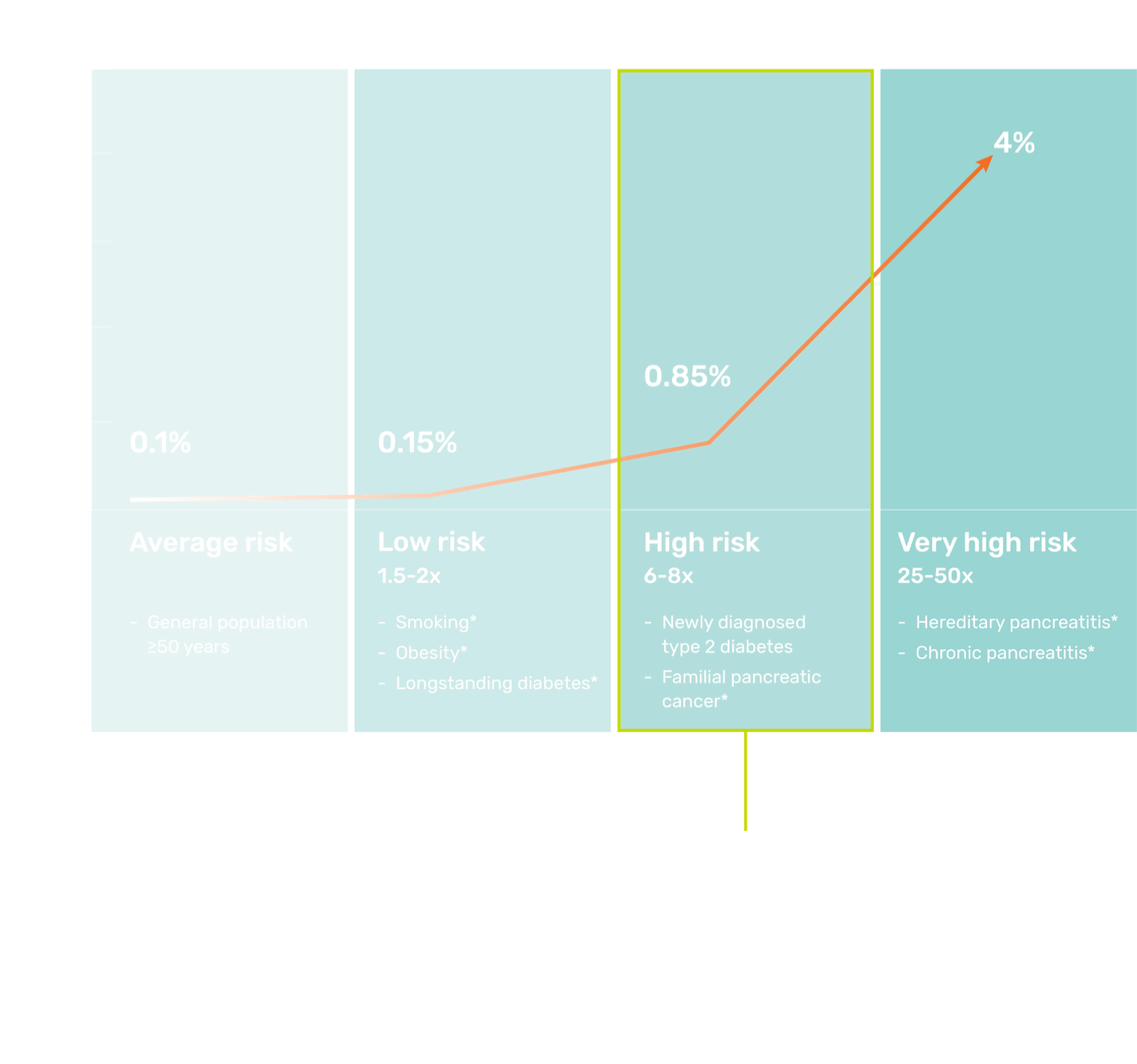
- Pancreatic cancer becomes more common with increasing age, with over 90% of cases in people over the age of 506,7
- Approximately 90% of pancreatic cancer cases are sporadic, with the remaining 10% having a genetic etiology2
According to guidelines from the American Gastroenterological Association, pancreatic cancer screening in high-risk individuals should begin at age 50, or 10 years younger than the initial age of familial onset.8
Prioritizing a significant high-risk population
Newly Diagnosed Type 2 Diabetes
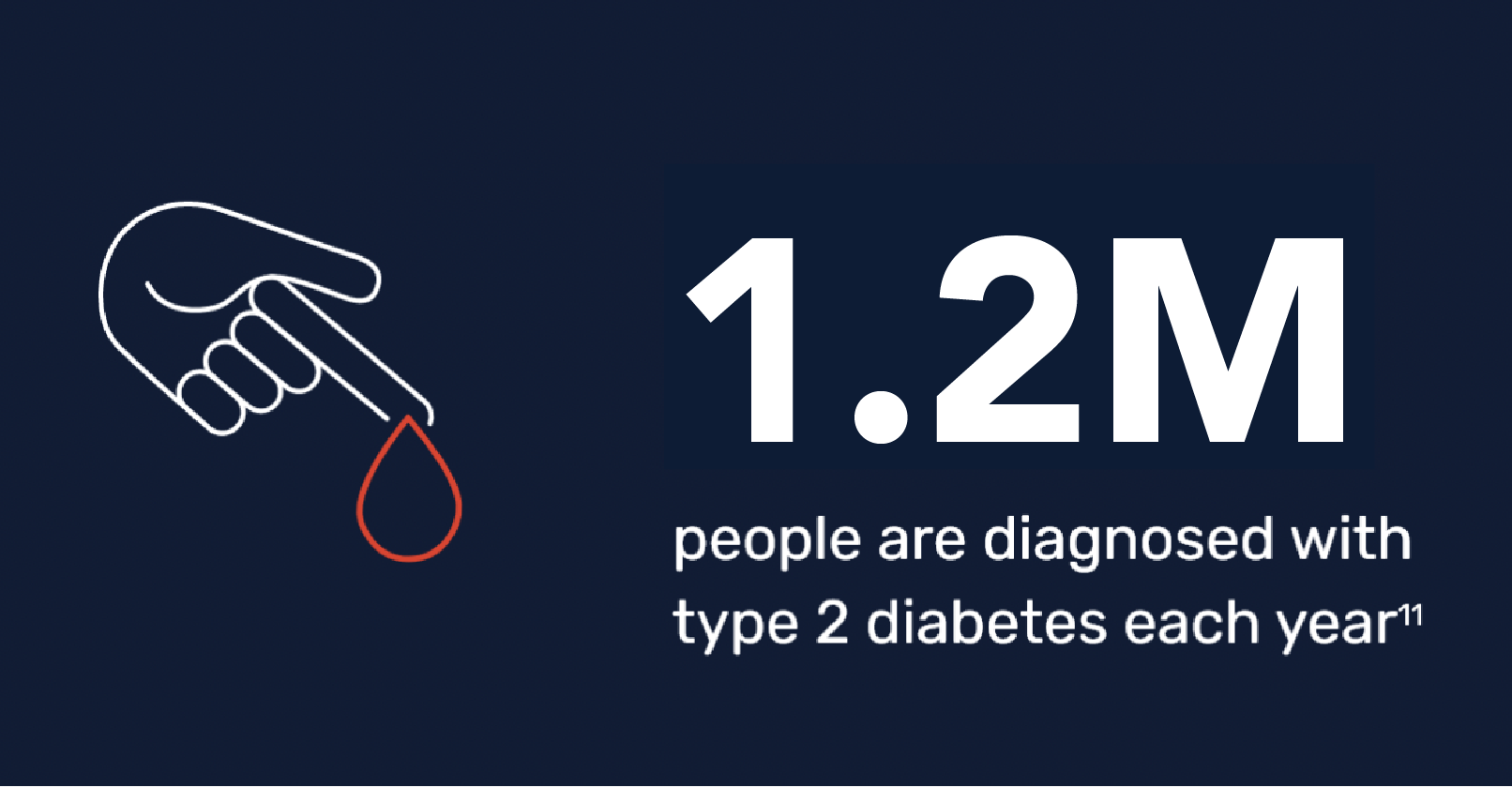
While diabetes has long been recognized as a risk for pancreatic cancer, there is emerging evidence of a critical link between pancreatic cancer and newly diagnosed (<3 years) type 2 diabetes in patients aged 50 and older.4,9,10
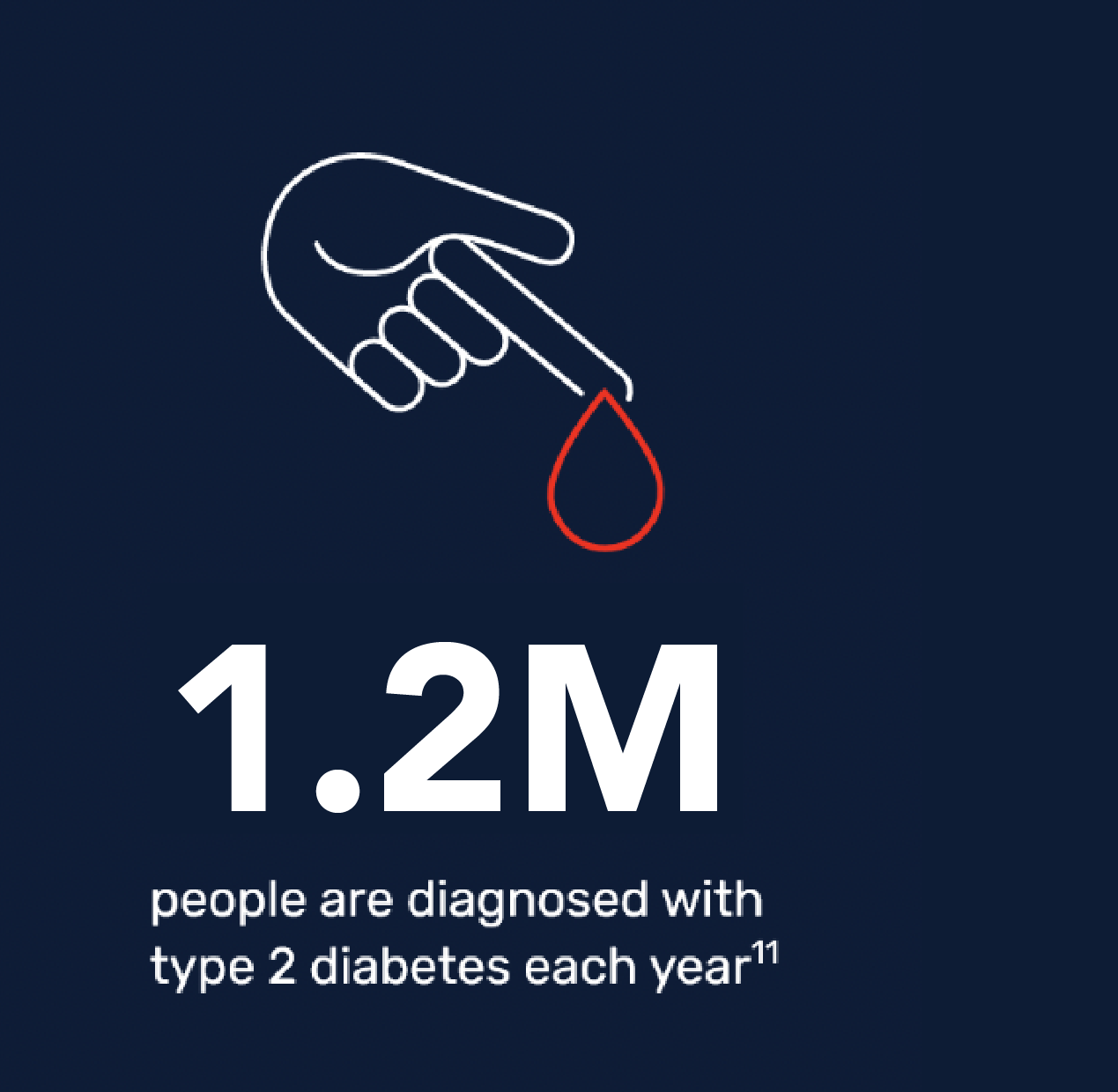

Recent studies of the pathogenesis of pancreatic cancer suggest that although longstanding diabetes (>3 years) increases risk and may play a causal role, new-onset diabetes actually may be a consequence of pancreatic cancer.12
How the Avantect test changes early pancreatic cancer detection
See how Avantect is changing the way pancreatic cancer is detected.

Important information
The Avantect Pancreatic Cancer Test is an early detection test. The test does not establish a diagnosis of pancreatic cancer, and results should be considered in the context of other clinical criteria. Definitive diagnosis of pancreatic cancer usually requires a series of imaging scans, blood tests, and a biopsy. Not all pancreatic cancers will be detected. Some patients with pancreatic cancer may have a “Signal not detected” result. Some patients without pancreatic cancer may have a “Signal detected” result. False-negative and false-positive results are possible. A “Signal not detected” result does not guarantee that no pancreatic cancer is present. In some cases, no result is obtained. While this is very uncommon, it may be caused by shipping delays or when there is not enough cell-free DNA for the test in the patient’s blood. If this happens, we generally ask for a repeat blood sample for testing at no extra cost.
The test was developed in the ClearNote Health CLIA-certified (CLIA# 05D2249973) and CAP-accredited (CAP# 9219174) laboratory and has not been cleared or approved by the US Food and Drug Administration (FDA).
References and notes
- Bengtsson A, Andersson R, Ansari D. The actual 5-year survivors of pancreatic ductal adenocarcinoma based on real-world data. Sci Rep. 2020;10:1-9.
- Pereira SP, Oldfield L, Ney A, Hart PA, Keane MG, Pandol SJ, Li D, Greenhalf W, Jeon CY, Koay EJ, Almario CV, Halloran C, Lennon AM, Costello E. Early detection of pancreatic cancer. Lancet Gastroenterol Hepatol. 2020 Jul;5(7):698-710.
- National Cancer Institute. Surveillance, Epidemiology, and End Results (SEER) Program. Cancer stat facts: pancreatic cancer (2012-2018 data). Available at: https://seer.cancer.gov/statfacts/html/pancreas.html. Accessed July 22, 2024.
- Blackford A, Canto MI, Klein AP, Hruban RH, Goggins M. Recent trends in the incidence and survival of stage 1A pancreatic cancer: a surveillance, epidemiology, and end results analysis. JNCI J Natl Cancer Inst. 2020;112(11):1162-1169.
- Chari ST. Detecting early pancreatic cancer—problems and prospects. Semin Oncol. 2007;34(4):284-294.
- National Cancer Institute. Surveillance, Epidemiology, and End Results (SEER) Program. Cancer stat facts: pancreatic cancer (2015-2019 data). Available at: https://seer.cancer.gov/statfacts/html/pancreas.html. Accessed October 27, 2022.
- American Cancer Society. Pancreatic cancer risk factors. Available at: https://www.cancer.org/cancer/pancreatic-cancer/causes-risks-prevention. Accessed October 22, 2022.
- American Gastroenterological Association. AGA guidance: when to screen for pancreas cancer. Available at: https://gastro.org/news/aga-guidance-when-to-screen-for-pancreas-cancer/. Accessed November 13, 2022.
- Sharma A, Chari ST. Pancreatic cancer and diabetes mellitus. Curr Treat Options Gastro. 2018;16:466–478.
- Chari ST, Leibson CL, Rabe KG, Ransom J, DeAndrade M, Petersen GM. Probability of pancreatic cancer following diabetes: a population-based study. Gastroenterology. 2005:129(2):504-511.
- American Diabetes Association. Statistics about diabetes. Available at: https://diabetes.org/about-us/statistics/about-diabetes#:~:text=New%20cases%3A%201.4%20m. Accessed July 22, 2024.
- Sah RP, Nagpal SJS, Mukhopadhyay D, Chari ST. New insights into pancreatic cancer-induced paraneoplastic diabetes. Nat Rev Gastroenterol Hepatol. 2013;10(7):423-433.